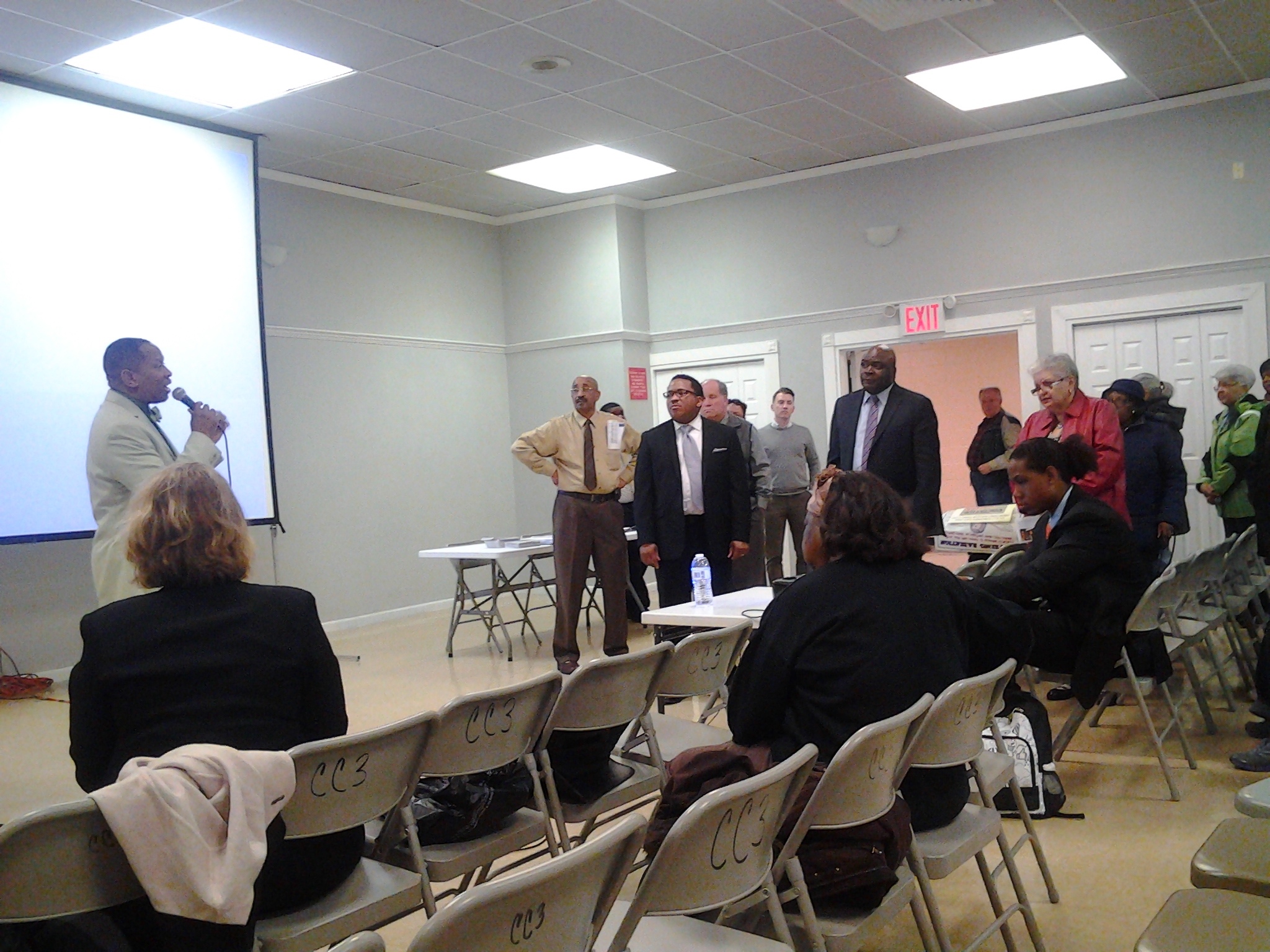
Last night, Council Member Andy King hosted a town hall meeting on health concerns in Co-op City at the commnity center on Einstein Loop. The focus was on Legionnaires’ disesase, of which there were 2 cases in the past year in the residential community.
https://www.youtube.com/watch?v=D5zv-y3fye0
 Sharon Balter, MD, of the Department of Health gave the presentation and explained the nature of Legionnaires’, a type of pneumonia, explained in detail below c/o the DOH. Balter was grilled by a number of local residents about the DOH’s actions in the matter, which requires the delicate dance of respecting private medical records while informing New Yorkers of public health concerns or potential concerns. The concensus of the Councilman and the audience was that recognizing that while pnuemonia is serious, Legionnaires’ should not be uniquely feared in the area and as long as one with pneumonia signs sees a physician, there is no public health risk.
Sharon Balter, MD, of the Department of Health gave the presentation and explained the nature of Legionnaires’, a type of pneumonia, explained in detail below c/o the DOH. Balter was grilled by a number of local residents about the DOH’s actions in the matter, which requires the delicate dance of respecting private medical records while informing New Yorkers of public health concerns or potential concerns. The concensus of the Councilman and the audience was that recognizing that while pnuemonia is serious, Legionnaires’ should not be uniquely feared in the area and as long as one with pneumonia signs sees a physician, there is no public health risk.
From the Department of Health:
What is legionellosis?
Legionellosis is an infection caused by a type of bacteria called Legionella. The disease has two forms:
- Legionnaires’ disease includes pneumonia and is the more severe form of infection.
- Pontiac fever is a milder, flu-like illness.
For data on legionellosis in New York City visit EpiQuery.
Why is it called legionellosis?
An outbreak of this disease in Philadelphia in 1976, largely among people attending a state convention of the American Legion, led to the name “Legionnaires’ disease.” Subsequently, the bacteria causing the illness was named Legionella, and the name for Legionnaires’ disease or Pontiac fever became legionellosis.
How widespread is legionellosis?
Each year, between 8,000 and 18,000 people are hospitalized with Legionnaires’ disease in the U.S. However, many infections are not diagnosed or reported, so this number may be higher. Cases occur sporadically and in outbreaks. More illness is usually found in the summer and early fall, but it can happen any time of year.
Where are Legionella bacteria found?
Legionella bacteria are found naturally in the environment, usually in water. They are found in rivers, lakes and streams worldwide in low numbers. However, most cases of legionellosis can be traced to man-made water systems where conditions are favorable for Legionella to grow in large numbers. Examples of such systems are whirlpool spas, hot tubs, humidifiers, hot water tanks, large plumbing systems, cooling towers and evaporative condensers of large air-conditioning systems. The bacteria grow best in warm water (77-108°F). Stagnation and the presence of scale, sediment, biofilm (a collection of microscopic organisms that sticks to the inner surface of pipes) and amoebae (microscopic organisms that provide nutrients for Legionella), also helpLegionella to grow. They do not seem to grow in car or window air-conditioners.
How does a person get legionellosis?
A person who has legionellosis most likely breathed water mist containing Legionella bacteria. The mist droplets must be small enough to be breathed into the lungs. Misting can be produced by large air handling systems in buildings, and by sprayers and other aerosol-producing devices. People may be exposed to mists in homes, workplaces, and public places. One example might be breathing in mist from a whirlpool spa that has not been properly cleaned and disinfected.
Risks for disease depend on how much bacteria is present in the water mist, how much a person breathes in, and individual health factors. Some cases of legionellosis are not completely understood. Legionnaires’ disease most often affects middle-aged and older people, particularly those who smoke or have chronic lung disease (like emphysema). People with weakened immune systems from cancer, kidney diseases, diabetes, or untreated AIDS, and people who take drugs to suppress the immune system (for example, after a transplant operation or chemotherapy) are also at higher risk.
Pontiac fever affects otherwise healthy persons.
Is legionellosis contagious?
No. legionellosis cannot be passed from person to person. Outbreaks of legionellosis have occurred when affected persons inhaled mists from a common water source contaminated with Legionella bacteria. Most cases of Legionnaires’ disease are isolated and not associated with outbreaks.
What occupations are at risk for legionellosis?
Little is known about legionellosis in the workplace. However, workers who operate aerosol-producing equipment or maintain air-handling units containing the bacteria may be at higher risk.
What are the usual symptoms of legionellosis?
Legionnaires’ disease can have symptoms like many other forms of pneumonia, so it can be hard to diagnose at first.
Symptoms of Legionnaires’ disease can include: fever, chills, and cough. Other symptoms are: muscle aches, headache, tiredness, loss of appetite, confusion and, occasionally, diarrhea. Chest x-rays usually show pneumonia. Symptoms usually appear 2 to 14 days after exposure to Legionella bacteria.
Symptoms of Pontiac fever include: fever, flu-like symptoms, and muscle aches. However, there is no pneumonia. Illness begins a few hours to two days after exposure. Patients generally recover in 2 to 5 days without treatment.
How is legionellosis diagnosed?
Diagnosis of Legionnaires’ disease and Pontiac fever requires special tests not routinely performed for people with pneumonia or fever. A doctor must consider the possibility of legionellosis to order the right tests. The most useful tests detect the bacteria in sputum or find Legionella antigens in urine samples. Another test compares antibody levels to Legionella in two blood samples obtained 3 to 6 weeks apart.
How serious is legionellosis and what is the treatment?
Legionnaires’ disease can be very serious and can cause death in 5% to 30% of cases. Most cases can be treated successfully with antibiotics, and healthy people usually recover from the infection.
Pontiac fever requires no specific treatment.
Does the New York City Health Department track cases of legionellosis?
Yes. The New York City Health Department requires doctors to report all cases of legionellosis. All cases are investigated to confirm diagnosis and to collect information on potential exposures. If an outbreak occurs, the New York City Health Department investigates possible environmental sources.
How can Legionella bacteria be controlled in building water systems?
The most important way to prevent legionellosis is to maintain cooling towers and plumbing systems to limit the growth and spread of Legionella bacteria. Visual inspection and periodic maintenance of building water systems is highly recommended.
Some best management practices for building water systems include:
- Maintain cold water below 68°F and heating hot water between 122°F and 140°F. Take care to maintain hot water faucet temperatures at no more than 120°F to prevent scalding.
- Drain, clean and disinfect hot water storage tanks and cooling towers at least once per year.
- Maintain a daily operation and maintenance manual that includes written details about repair, alteration, operating time, monitoring and inspection and the use of anti-corrosives, biocides and disinfectants.
- Document all operations and maintenance activities in a log book.
- Treat circulating water systems to control microorganisms, scale, and corrosion. Contact equipment manufacturer for information about biocides or rust inhibitors appropriate to your systems.
- Inspect piping systems to ensure full recirculation loops. Remove any “dead ends” or capped lines. Dormant or unused piping should be thoroughly disinfected and flushed before placing back in service.
For Additional Information
Visit the Centers for Disease Control and Prevention (CDC) Legionellosis Resource Site











Follow Us